January 30/31, 2018
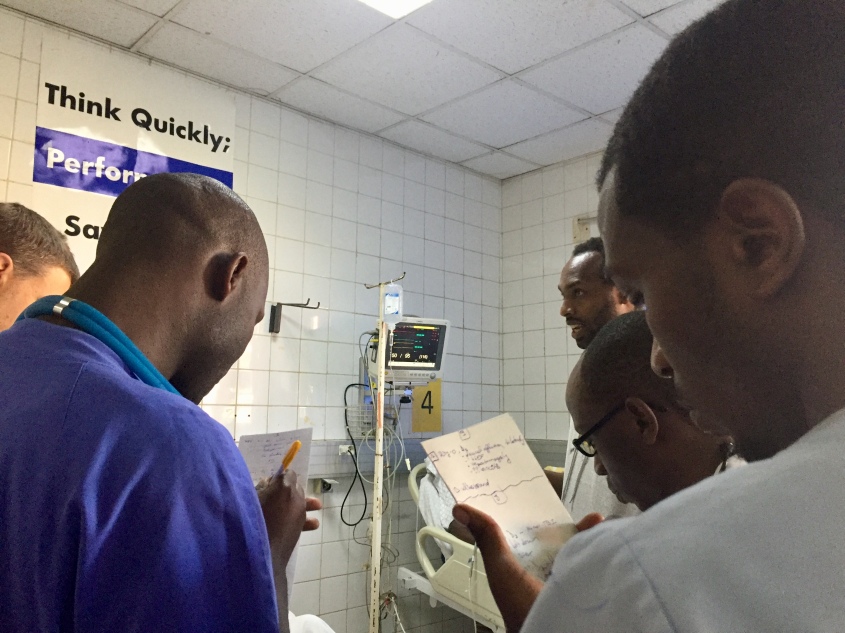
This morning we returned to the Lemigo Hotel for the last day of the trauma course taught by the students we trained last week. It was again inspiring to see these new educators helping to expand SAMU and improve trauma care throughout Rwanda. The goodbyes were difficult knowing I won’t likely come back to Rwanda. My husband, Amir, will hopefully be making the next trip towards the end of April if things go as planned. I’m excited for him to meet these wonderful people and share some of the same moving experiences. Travel is something we love to do together. In this case we are both sharing a travel experience, just 3 months apart.
The end of a trip is always a time for reflection. Interestingly, my goals in keeping this daily travel journal have expanded since I first started. Day 1 I was trying to capture my observations for the benefit of my own memory and perhaps to help educate my daughter. But what I found through the power of social media, was that the audience wanting to learn about Rwanda, SAMU and the efforts by VCU was much larger. As each day drew to a close, and I struggled to do justice to the beauty and energy of Rwanda with my photos and writing, I somehow received more feedback, more questions, more people engaged in learning about this unique place.
In full disclosure, I have chosen to make some edits to my earliest posts. As I learned more about the culture, tradition and pride of Rwandans, I realized that as a guest invited to their country, I wasn’t always respectful of that invitation. I haven’t written anything untrue, just adjusted my perspective and henceforth my words. Trust is a difficult thing for Rwandans (as expected when neighbors turn on neighbors), and I just want to give it due respect.

One of my major goals both personally and professionally was to understand Rwanda’s EMS system. I’ve written much about the training, equipment and staffing, but only briefly mentioned how their 912 (911) system functions. Mobile phones aren’t widely available in rural areas of Rwanda. The country has designated a team of laypeople as citizen responders throughout these regions. When someone requires 912, they often do not have a phone with which to call. Instead, they physically go to the citizen responder who does have a mobile and that person dials 912. As described in my Day 2 post, the call is answered by one to three individuals (staffing is variable) who have a single mobile phone that rolls to a single backup should the first be busy. Calls are tracked in an Excel spreadsheet where data is manually entered and then the information ultimately filed away by day. Ambulances do not call the hospital directly, rather they call the 912 dispatcher to provide their patient report. This can be problematic for many reasons. The 912 dispatchers vary in their medical training, anywhere from no medical training to Nurse Anesthetist. So, it is possible that a patient report could be called to a dispatcher without medical training, who then has to call the charge nurse at the receiving hospital to relay that information. It’s literally the telephone game.
Additionally, there is no formal process for online medical direction. Since the ambulances don’t speak with the nurses or doctors at the hospital, they can’t easily call and ask them questions or request orders. In speaking with many of the SAMU staff, often individual providers will have relationships with certain doctors and happen to have their mobile number. One nurse anesthetist described a case where a man had suffered a spinal injury during a motor traffic accident (MTA). On physical exam, he had an obvious step-off deformity of his thoracic spine and no movement in his lower extremities. Unclear how to safely immobilize him given the severity of the step-off, she dialed up the Neurosurgeon directly for guidance.
Everyone I spoke to had at least one story where they called a doctor directly to ask a question. But, if you are new or just don’t know the right specialist, you are on your own. Given the severity of injuries and frequency of polytrauma in this system, I feel bad these guys are out there doing it on their own, without the support of online medical direction. It’s a testament to their professionalism and ingenuity that they can do what they do without that support. The good news is that in speaking with the SAMU leadership, dispatching, online medical direction and protocols are a top priority for development. There are plans in place for SAMU to borrow best practices in dispatching from the Richmond Ambulance Authority, and work is underway to modify the ODEMSA protocols to fit the needs and challenges of Rwanda. After all, if you’ve seen one EMS system you’ve seen one EMS system.

Somewhat off-topic but of interest (at least to me), is the continuing education (CE) process for medical staff at all levels in Rwanda. Just like the US, Rwanda has category 1 and 2 requirements, with credits granted in 1 hour time blocks. Ahead of our trip, Dr. Sudha spent significant time working with the Ministry of Health to ensure our Trauma Care Course met all continuing education requirements for the nurses, nurse anesthetists and doctors taking our course. After passing the final exam for the course, students received a certificate of completion and an official government stamp in their CE books. The Medical, OB/Neonatal and Pediatrics courses the team will return to teach later this year will also count towards CE for the SAMU staff. Now if only it counted for physician or EMS CE for me.
Lastly, there’s something that’s been haunting me since visiting the Genocide Memorial. I’m the first to admit that unlike my husband who can recite dates and motives for every international conflict since the existence of man, I am not a history buff. Like most, I knew of various genocides throughout history, but I had never taken the time to truly understand how a nation and its people propel towards that tipping point. In visiting the Genocide Memorial, you see how the two ethnic groups at the time in Rwanda, Hutu and Tutsi, suffered under a systemic campaign to pit one group against another and eradicate the Tutsi. It didn’t happen overnight but rather over years.
Propaganda, which as a child of the 80s growing up during the cold war, I thought of as a Soviet, communist tool, filled the radio airwaves and newspapers across Rwanda. In April of 1994, I was finishing my sophomore year in high school. Privileged to attend one of the best public schools in Virginia, my biggest worries were whether or not Pearl Jam was going to break up, and how to best prep for my PSAT. Across the globe in Kigali, someone was importing thousands of machetes and distributing them to the Hutu, all while the government spread a message of hate and violence.

In one compelling exhibit, the Genocide Memorial features skulls of many of those killed, “hacked by machete” as the plaques read. Nearly all of the skulls have obvious fractures if not complete holes, the consequence of which is obvious, even to the untrained eye. Thousands of Rwandans, including babies and children, died from traumatic brain injury (TBI) during the Genocide. As I rounded this week in the hospital, I couldn’t help but note how TBI (now mostly from MTAs) still plagues this country. I felt like I had PTSD – my mind flashing between the images of the Genocide, heads wrapped in makeshift bandages, and now patients in CHUK, heads wrapped in gauze.
As I expected to be the case, multiple people I met on this trip lost multiple loved ones during the Genocide. I’ve deliberately not told those stories by request for privacy, but please know that they are real. How someone can survive a Genocide, recover from losing nearly every member of their family, and then devote their lives to helping others… it’s overwhelming to think about.
I am leaving Rwanda feeling honored. Honored to teach such resilient and passionate people. Honored for the opportunity to see and learn about genocide at the Kigali Genocide Memorial. Honored to have met the survivors themselves – been entrusted with their stories, and seen first hand how you can rise to inspire others, even after you’ve lost all hope.
If you are ever lucky enough to travel to Rwanda, visit the Kigali Genocide Memorial. Head east to Akagera National Park to enjoy the animals. If you see an ambulance or find yourself in hospital, say “thank you” to the staff. When you meet a Rwandan, don’t ask if they are Tutsi or Hutu. It’s not that it will offend them, but rather it is a waste of your time. Every answer you get, from the President to the street sweepers, will be “I’m Rwandan.”
~Steph
Explore more days in Rwanda:
Rwanda Day 1 | Rwanda Day 2 | Rwanda Day 3 | Rwanda Day 4 | Rwanda Day 5 | Rwanda Day 6 | Rwanda Day 7 | Rwanda Day 8 | Rwanda Day 9